What is oral cancer?
Oral cancer is a type of cancer that affects the mouth (oral cavity) and the surrounding areas, such as the lips, gums, and throat. It can occur in any part of the oral cavity, including the tongue, the roof of the mouth (palate), and the inside of the cheeks. Oral cancer can be life-threatening if it is not detected and treated in its early stages. Some common symptoms of oral cancer include sores or growths in the mouth that do not heal, pain or difficulty swallowing, and changes in the way the teeth fit together when biting. Risk factors for oral cancer include tobacco use (smoking or chewing tobacco), heavy alcohol consumption, and a diet low in fruits and vegetables.
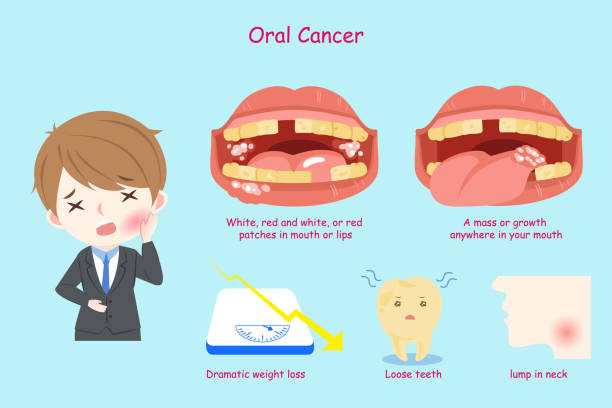
What are the signs and symptoms of oral cancer?
Here are some common signs and symptoms of oral cancer:
Sores or growths in the mouth that do not heal
Pain or difficulty swallowing
Changes in the way the teeth fit together when biting
Persistent bad breath
White or red patches on the gums, tongue, or lining of the mouth
Loose teeth or dentures that no longer fit properly
Pain or numbness in the mouth or lips
Swelling in the jaw or neck
Persistent earache
It's important to note that these symptoms can also be caused by other conditions, so it's important to see a doctor or dentist if you are experiencing any of these symptoms. They can perform a thorough examination and determine the cause of the symptoms.
How is oral cancer diagnosed?
Oral cancer is usually diagnosed through a combination of a physical examination, a review of the patient's medical history, and one or more of the following tests:
Biopsy: A biopsy involves removing a small sample of tissue from the suspicious area and examining it under a microscope to check for cancer cells. A biopsy is the only way to definitively diagnose oral cancer.
X-ray: An X-ray can help to show whether there are any abnormal growths in the mouth or throat.
CT scan: A CT (computed tomography) scan is a type of X-ray that produces detailed images of the inside of the body. It can help to show whether the cancer has spread to other areas of the body.
MRI (magnetic resonance imaging): An MRI uses a powerful magnet and radio waves to produce detailed images of the inside of the body. It can be used to help detect oral cancer and to see whether it has spread to other areas.
PET (positron emission tomography) scan: A PET scan is a type of scan that uses a small amount of radioactive material to produce detailed images of the inside of the body. It can be used to see whether the cancer has spread to other parts of the body.
If oral cancer is diagnosed, the healthcare provider will perform additional tests to determine the stage (extent) of the cancer. This will help to guide treatment decisions.
How is oral cancer treated?
The treatment of oral cancer depends on the stage (extent) of the cancer, the specific type of cancer, and the patient's overall health. Treatment options for oral cancer may include:
Surgery: Surgery is the most common treatment for oral cancer. The type of surgery will depend on the location and size of the cancer. It may involve removing the cancerous growth and some of the surrounding healthy tissue (resection), or it may involve the removal of part or all of the affected organ (such as the tongue or jaw).
Radiation therapy: Radiation therapy uses high-energy beams, such as X-rays, to kill cancer cells. It may be used in combination with surgery or as a standalone treatment.
Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be used in combination with surgery or radiation therapy, or as a standalone treatment.
Targeted therapy: Targeted therapy uses drugs to target specific proteins or genes that are involved in cancer cell growth and division. It may be used in combination with chemotherapy or as a standalone treatment.
It's important to note that treatment for oral cancer can be complex and may involve a combination of the above treatments. A healthcare team that includes an oncologist (a cancer specialist), a surgeon, and a radiation oncologist will work together to develop the most appropriate treatment plan for the individual patient.
What are the risks and benefits of oral cancer screening?
Oral cancer screening is the process of looking for signs of cancer in the mouth before symptoms develop. It is typically done by a dentist or other healthcare provider during a routine checkup. Some possible benefits of oral cancer screening include:
Early detection: Oral cancer screening can help to identify cancer in its early stages, when it is most treatable.
Treatment options: If oral cancer is detected early, there may be more treatment options available, and these treatments may be more effective.
Improved survival: Early detection and treatment of oral cancer can improve the chances of survival.
There are also some potential risks and limitations to oral cancer screening:
False positives: Oral cancer screening tests can sometimes produce false positive results, meaning that they suggest cancer is present when it is not. This can lead to unnecessary anxiety and additional testing.
False negatives: Oral cancer screening tests can also produce false negative results, meaning that they suggest cancer is not present when it is. This can delay the diagnosis and treatment of cancer.
Invasive procedures: Some oral cancer screening tests may involve invasive procedures, such as biopsy, which carry a small risk of complications.
Overall, the benefits of oral cancer screening are likely to outweigh the risks for most people. However, it is important to discuss the potential risks and benefits with a healthcare provider and to consider individual factors, such as the risk of developing oral cancer and the potential for harm from false positive or false negative results.
What are the long-term risks and effects of oral cancer?
Oral cancer can have serious long-term effects, both physically and emotionally. Some potential long-term risks and effects of oral cancer include:
Disfigurement: Surgery to remove cancerous tissue can result in disfigurement, such as the loss of part of the jaw or tongue. This can affect appearance and speaking ability.
Dysphagia: Surgery or radiation therapy to the head and neck area can cause difficulty swallowing (dysphagia), which may require the use of a feeding tube.
Dry mouth: Radiation therapy to the head and neck area can cause dry mouth (xerostomia), which can lead to tooth decay and other oral health problems.
Neuropathy: Some chemotherapy drugs can cause nerve damage (neuropathy), which can result in numbness, tingling, or pain in the hands and feet.
Emotional effects: Coping with cancer and its treatment can be emotionally challenging and can affect mental health. Support from family and friends, as well as counseling and support groups, can be helpful in addressing these issues.
It's important to note that not all patients will experience these long-term risks and effects, and the severity of these effects will vary from person to person. Working with a healthcare team can help to minimize the potential risks and effects of oral cancer treatment and to manage any side effects that do occur.


Post a Comment